Chronic kidney disease (CKD) and chronic renal failure (CRF) are interchangeable terms that describe progressive kidney damage and reduced kidney function in dogs and cats. Prevalence is low in the general pet population, but rises significantly with age, and is more commonly seen in older cats than dogs. An estimated 30% to 50% of cats who reach 15 years of age will develop CKD.
Once you notice your pet’s clinical signs, CKD has already progressed to an advanced stage that may not respond to treatment. The Adamson Veterinary Services team knows that early CKD detection leads to more effective treatment and a longer life expectancy, so we provide advanced diagnostic testing to achieve this goal.
Pet CKD causes
Kidney damage and subsequent CKD can occur in any pet, but is far more common in older pets. An underlying cause is never found in most cases, but a few pets may have diseases that led to their CKD, including:
- Congenital kidney malformations
- Infections
- Inherited conditions
- Cancer
- Immune-mediated diseases
- Clotting disorders
Pet CKD signs
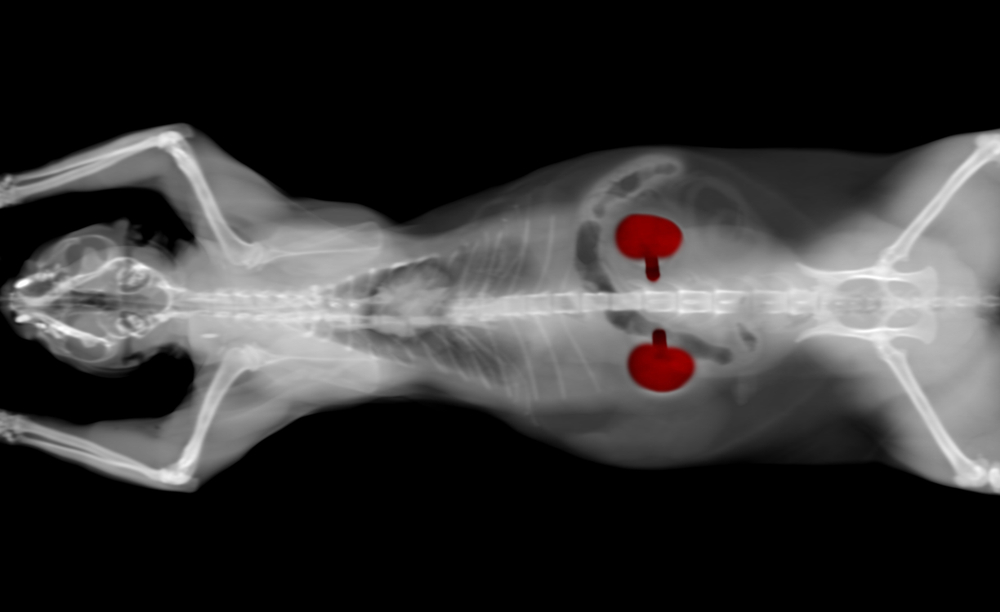
The kidneys filter waste products from the blood, concentrate urine, regulate electrolyte levels, and assist with red blood cell production through complex hormonal mechanisms. The first CKD sign is often dilute urine, which pet owners may or may not notice at home. As CKD progresses, other signs will appear or worsen, including:
- Increased thirst and urine volume
- Decreased appetite
- Nausea or vomiting
- Weight loss
- Bad breath
- Lethargy
- Dehydration
- High blood pressure, which may lead to eye damage or blindness
Pet CKD diagnosis
Traditional CKD diagnosis relies on tests that measure blood toxin levels, as well as urinalysis, which is necessary to evaluate urine concentration, check for infection, and determine whether protein is leaking from the bloodstream into the urine. Changes to urine concentration are usually the first CKD sign, but may occur in conjunction with blood changes.
Blood urea nitrogen (BUN) and creatinine are the main blood components that indicate kidney function. Creatinine is the more sensitive value and usually slowly creeps up as CKD progresses, but may remain in the “normal” laboratory reference range during early disease stages. Creatinine levels can also be impacted by hydration and other disease states, making them challenging to interpret. Therefore, early CKD stages can be easy to miss, and treatment is delayed. Because CKD responds best to earlier treatment, a new test called symmetric dimethylarginine (SDMA) was developed.
The impact of early CKD detection in pets
SDMA is better correlated with kidney function than creatinine and is not impacted by other diseases, which means the test is more stable over time and can detect changes earlier than other tests. We include SDMA with all our send-out blood chemistry panels and wellness profiles, so we can watch for trends and small changes across your pet’s lifetime. As soon as a pet’s SDMA becomes elevated, we can implement treatment strategies while CKD is still in early stages.
CKD severity is graded from stages one through four, and until SDMA became available, most CKD was detected during stages two, three, or four. SDMA can detect stage one, while the kidneys still maintain some functionality, and beginning treatment in this early stage can protect remaining kidney cells and preserve function for months or years. Treatment that does not begin until later stages is less effective, because the damage has already been done.
Pet CKD treatment options

Early CKD can be managed with a special diet and increased fluid intake. The diet restricts protein and balances minerals and electrolytes to reduce the kidneys’ workload. Feeding this diet in a canned form or offering fresh, running water can encourage your pet to take in more fluids.
Advanced CKD stages are more difficult to treat and require more time and expense. In addition to a special diet and strategic nutritional support, these pets may require:
- Blood pressure medication — This medication controls blood pressure and reduces urinary protein loss.
- Subcutaneous fluids — Most pets in advanced CKD cannot maintain adequate hydration, which makes them feel sicker. Fluids can be given at home through a needle placed underneath the skin.
- Anti-nausea medications — Increased blood toxins can lead to nausea, poor appetite, and weight loss, which these medications can reverse or improve.
- Supplements—Some pets with CKD are missing potassium or have too much phosphorus, which supplements can correct.
The best way to protect your pet from CKD is disease detection in the early stages through regular wellness examinations and blood tests. If your pet has not had their annual appointment this year, contact Adamson Veterinary Services to schedule a comprehensive wellness and preventive care visit.






Leave A Comment